What is DME Medical Billing

What is DME billing?
Think of DME billing, also known as DME operations, as the bridge between patients who need medical equipment at home and the reimbursement that makes it financially possible. Wheelchairs, CPAP machines, continuous glucose monitors - these aren't one-time purchases made in a doctor's office. They're long-term medical devices that patients use at home, and getting paid for them involves a completely different process than standard physician billing.
The documentation requirements are more detailed. The compliance guidelines are stricter. Medicare, Medicaid, and private insurers each have their own specific coding protocols that providers need to follow.
Summary
DME billing covers reimbursement for long-term, home-use medical equipment and is more complex than standard physician billing. It demands detailed, payer-specific documentation, accurate HCPCS Level II coding with modifiers, and steps like eligibility verification, prior authorization, and ongoing compliance. The workflow spans prescription and intake through coding, submission, and follow-up, with timelines varying by payer. Denials often stem from documentation and authorization gaps; strong protocols, staff training, and AI-enabled tools (e.g., automated intake and compliance checks) improve first-pass rates and speed revenue.
Why is DME billing different from other medical billing?
Physician services usually work on a straightforward fee-for-service basis. You provide a service, you bill for it, you get paid. DME operations? Not so simple.
Before you can even deliver equipment, you may need preauthorization. Detailed proof that the equipment is medically necessary is needed. And the compliance documentation doesn't stop once you've been paid - it's an ongoing cycle for continued use of equipment.
The documentation standards are stricter than what you'd see in a typical medical practice. You'll need payer specific forms, insurance payers audit DME claims more frequently, and there's also a rental-versus-purchase decision, which follows complex protocols that vary by equipment type and payer.
On top of all that, regulations change constantly. Accreditation standards must be maintained.
What documents are needed for DME billing?
Missing a single document can derail your entire claim. Although documentation requirements vary by product and payer, below are a few of the many requirements:
A valid physician's prescription isn't enough on its own - it requires detailed specifications. A Standard Written Order (SWO) or Written Order Prior to Delivery (WOPD) is also needed. Additionally, patient demographics, insurance information, product specific documentation such as a sleep study, and proof of delivery must be complete and accurate.
Medical records that justify why the patient needs this specific equipment. Itemized invoices showing equipment costs. When applicable, signed advance beneficiary notices (ABNs). Prior authorization approvals from the insurance company.
Even one missing signature or one incomplete form could result in a denied claim and delayed reimbursement.
Coding Systems Used in DME Operations
HCPCS Level II codes are the backbone of DME billing. These alphanumeric codes specifically identify durable medical equipment, prosthetics, orthotics, and supplies. They start with a letter (usually A, E, K, or L for DME items) and end with four digits.
Getting the code right matters more than you might think. Billing staff need to understand modifiers - those additions that tell the whole story. Is this equipment rented or purchased? New or used? Is it replacing existing equipment? Left or right laterality? Each of these details require a specific modifier.
How does DME coding help with billing?
Accurate coding tells payers exactly what equipment was provided and why it was medically necessary. When your coding is precise, several things happen: claim rejections drop, payments process faster, and audit risks decrease.
Modern DME billing programs have changed the game. Built-in code validation catches errors in real time, eligibility verification happens instantly, and automated compliance checks identify problems before claims ever leave your office.
The result? Higher first-pass claim acceptance rates and better revenue cycle performance overall.
Steps to Submit an Insurance Claim for DME
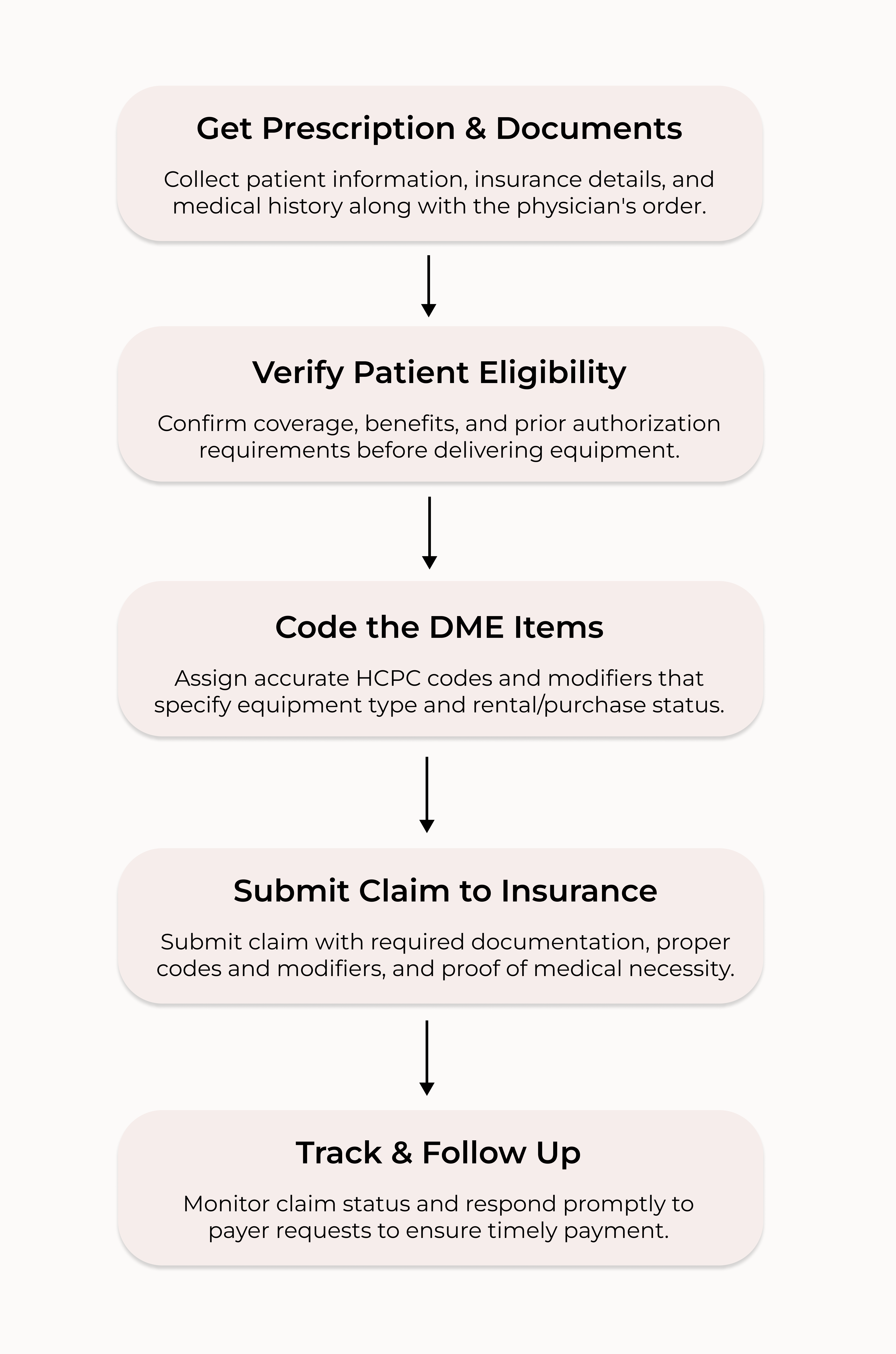
Getting the prescription and documents
Everything starts with a physician determining that a patient needs DME. The prescribing doctor writes an order that includes the necessary equipment, the medical diagnosis, how long the patient will need it, as well as their signature and credentials.
Then DME suppliers step in to collect all necessary information to fill the order. Insurance coverage details, demographic data, relevant medical documentation - all of it matters. This initial phase is one of the top reasons claims get denied - incomplete information is a huge challenge.
Checking Patient Eligibility
The next step is to verify coverage. Confirming the patient has active coverage before delivery is crucial. Check what their specific benefits cover and what limitations apply. Determine any out of pocket or deductible amounts, and communicate this with the patient to ensure they understand and approve of the cost. Identify whether prior authorization is required.
Real-time eligibility verification tools have made this step seamless. Coverage status and benefit details are instantly verified, which protects both the provider and the patient from surprise costs down the road.
Coding the DME Items
After eligibility is confirmed, billing specialists assign the appropriate HCPCS code to each piece of equipment. This takes detailed knowledge - not just of the codes themselves, but how they apply to different equipment types, medical conditions, and coverage scenarios.
Then come the modifiers. Rented or purchased? New or used? Replacement equipment? Getting the coding right at this stage helps your claim get paid correctly the first time. If the coding is incorrect, you're looking at hours of rework and resubmission as well as compliance and audit concerns.
Sending the Claim to Insurance
Claims go out to the insurance payer with everything attached: required documentation, proper codes and modifiers, detailed charge itemization, and supporting documentation for medical necessity.
Getting Paid and Following Up
Once your claim is submitted, the payer reviews it for accuracy, medical necessity, and coverage compliance. Clean claims typically take 14 - 60 days to process. Complex cases can take longer.
Actively monitoring claim status, responding quickly when payers request additional information, and following up on unpaid claims is critical to cash flow.
It depends on the payer and how complex the claim is.
Medicare typically processes clean electronic claims in 14 - 30 days. Private insurance companies take 30 - 45 days on average. Medicaid varies wildly by state and can be anywhere from 30 to 90 days.
Those timelines assume everything is complete and accurate: no errors, complete documentation, no questions about medical necessity. Claims requiring additional information or medical review can take significantly longer. Implementing best practices in documentation and using advanced DME billing automation can substantially reduce processing times and improve cash flow.
Common Challenges in DME Operations
Documentation issues cause more claim denials than anything else. Incomplete physician signatures on prescriptions or unsigned medical records are small mistakes with big consequences.
Some other common challenges include prior authorization delays, which can hold up equipment delivery and reimbursement. Coverage rules are complex and vary between payers.
Maintaining the specialized expertise to handle all this is where many DME billing companies struggle.
How can healthcare providers reduce billing denials?
Prevention beats correction every time.
Put documentation protocols in place so all required information gets collected before equipment goes out the door. Train your staff thoroughly on current coding requirements and payer-specific rules - and keep that training current.
Billing software with built-in compliance checks and real-time eligibility verification helps to catch problems before they become denials. A proactive denial management process tracks why claims get denied, identifies patterns, and implements changes before small issues turn into systemic problems.
Why Do DME Claims Often Get Denied?
DME claims get denied more often than other types of medical billing because they're more complex and the regulatory requirements are stricter.
Technical denials happen frequently - patient eligibility issues, coordination of benefits errors, missed timely filing deadlines. DME billing software catches many of these errors before submission, which helps keep your revenue cycle healthy.
How AI and Automation Help Avoid Denials and Increase Revenue
AI technology has changed what's possible for DME. Issues get identified early, rework drops, first-pass success rates climb, and reimbursements accelerate.
Notable Systems helps DME providers transform messy medical documents into clean, billable data - operations get streamlined and reimbursements flow more steadily.
Order Intake captures inbound documents from fax, email, mail, and other sources, then processes them instantly within your existing workflows. This solution automatically identifies and classifies documents - even handwritten or unstructured ones. Patient information, provider details, payer data, diagnosis codes are all extracted accurately. Customized rules check for completeness and flag issues like missing dates of birth or mismatched codes before anything reaches your billing systems.
Payor Greenlight System (PGS) runs real-time compliance assessments based on specific payer reimbursement criteria. Claims get checked for medical necessity and compliance before submission. Providers spot issues early and reduce rework. First-pass success rates improve. Claims move through faster without requiring bigger billing teams. Fewer denied claims mean less back-and-forth, which frees up your team to focus on care and operations instead of reprocessing.
These AI-powered solutions accelerate order processing, help avoid denials, minimize write-offs, and demonstrate accuracy during audits and appeals. Overall, patients get faster results and your time to revenue shrinks.
Ready to optimize your DME operational process?
Understanding DME operations is the starting point. Whether you strengthen your internal capabilities or partner with a specialized DME medical billing company, the right investment in processes, training, and technology makes all the difference in maximizing reimbursement and maintaining compliance in this complex segment of healthcare. Book a demo to learn how Notable Systems can streamline this process.
